最近看到不少自媒体在转发一篇标题为“NMN要黄了”、“不老神药要塌了”的文章,这篇文章援引一篇4月30日发表在《细胞·代谢》上的研究[1],研究确实是一篇新研究,但部分自媒体解读得实在离谱。
有多离谱呢?不客气的说,把这篇研究解读成“NAD+无用论”完完全全就是误读,这篇论文既没有提出这个观点,同时研究者在论文中也没有提出任何类似的观点。
长寿之家Changshou.com的专家团队在仔细研究了这篇论文和研究者引用的一些相关论文后,我们认为上述文章的标题和结论都带有多个不实信息,误导了公众的理解。
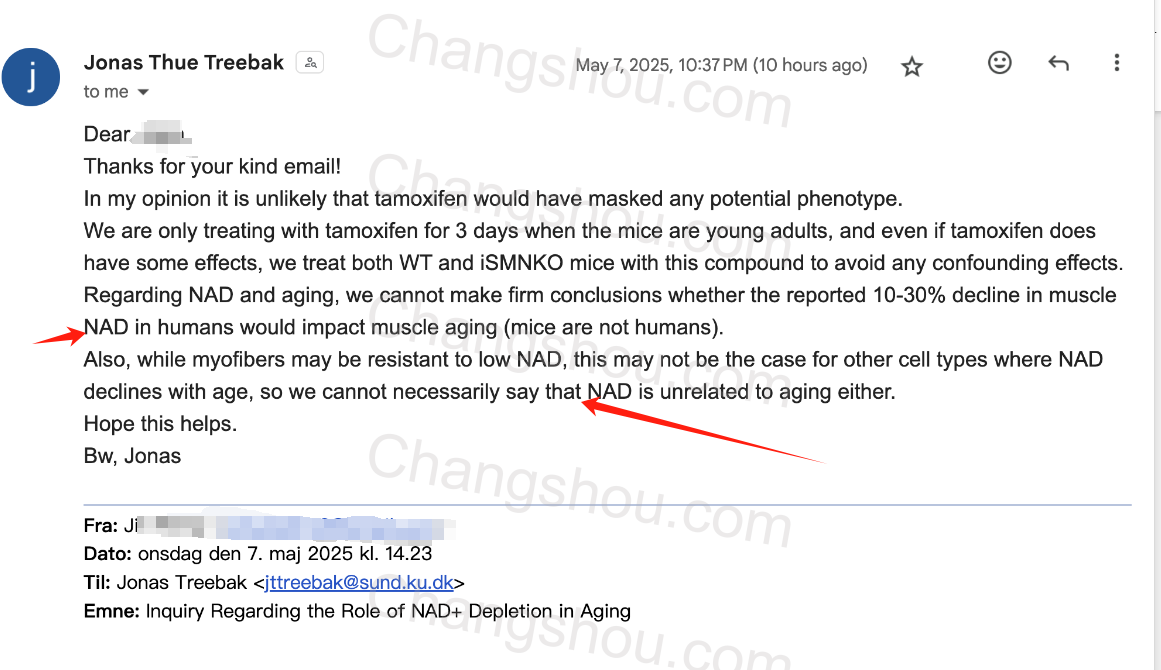
为了确认我们的理解没有问题,我们特意向本文的通讯作者,约纳斯·特雷拜克(Jonas T. Treebak)博士致函咨询。
特雷拜克博士于丹麦时间5月7日回复了长寿之家Changshou.com,在回复中,他明确表示:“我们无法得出NAD+和衰老无关的结论”。
下面就让我们用真正科学的态度,来审视这项研究到底说了什么?
真相:研究者没说过“补充NAD+在浪费钱”
知乎有一个经典的说法叫“先问是不是,再问为什么”,这句话也同样适用。
在上述自媒体报道中,有提到“研究团队发现,补充NAD是在浪费钱……”这样的词语,但我们反复翻阅论文全文,也没有提到任何关于“浪费钱”的表述。
稍稍动脑也可以得出结论,一个发布在《细胞》子刊的,针对小鼠的代谢研究,怎么也不会跟“浪费钱”这个观点挂上钩。
其次,上述自媒体还在标题处指出“NAD+水平下降没有加速衰老、不会损害代谢”——很抱歉,原论文也没有提到这句话。
本研究的标题是《骨骼肌中 NAD 的消耗不会损害肌肉功能或加速衰老》,研究只讨论了骨骼肌NAD+水平的变化,并没有提到其他器官的NAD+变化,结论是针对骨骼肌的NAD+耐受性。
上述自媒体本质上使用了一种偷换概念的手段,就像发现“人少个指甲也能活”,就推论“所有器官都不重要”一样荒谬。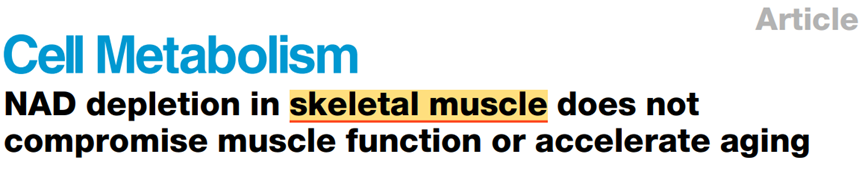
当然,作为一篇发布在《细胞》子刊的研究,研究者本身的成果是经过大量实验与同行评议的,这篇研究本身对于NAD+相关的代谢研究也有重大意义。
我们想讲的是,我们应该如何向普通人解读一项科研成果?以及,为什么这个研究不能否定NAD+的价值?
长寿之家Changshou.com将从实验设计的局限性、NAD+合成代谢最新进展、现有人类临床证据等多个角度,深入分析这项研究,并澄清常见的误读。
研究解读:这项研究到底做了什么?
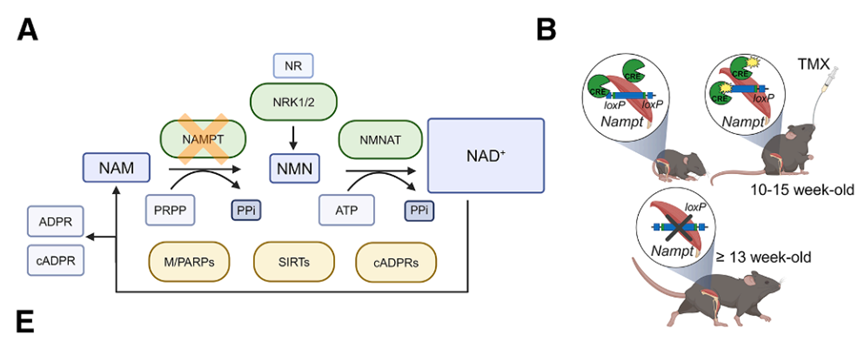
研究采用了特定的小鼠模型,即诱导型骨骼肌特异性NAMPT敲除小鼠(ISMNKO)。
如果你阅读过长寿之家Changshou.com此前关于NAD+体内合成路径的文章,那一定知道NAMPT是NAD+补救合成通路的关键酶,研究者此举是通过基因敲除技术,“清除”了肌肉中通过补救途径合成的NAD+,使得肌肉中的NAD+水平骤降85%。
他的结果显示,尽管NAD+下降,小鼠的肌肉力量、线粒体功能和运动能力都没有受到显著影响,老年小鼠的转录组、蛋白质组和线粒体特征也未改变,肌肉衰老没有加速。
这一结论似乎挑战了过去认为“NAD+下降直接导致肌肉功能衰退”的观点。
为什么说“似乎挑战了过去的结论”。是因为在2016年同样发表在《细胞·代谢》上的一项研究中,和这篇文章的研究思路非常相似,但却得出了相反的结论,该研究认为,在骨骼肌中敲除NAMPT,会导致肌肉严重退化[5],这是为什么?
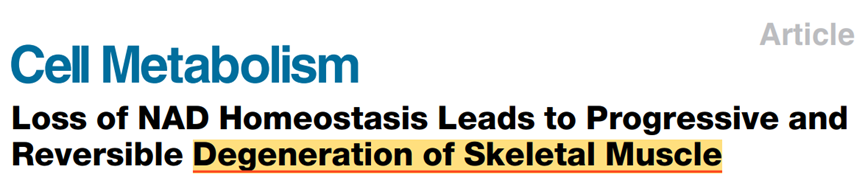
2025年的这篇论文的研究者也讨论了这个差异,他认为两者的差异主要在于小鼠模型的不同。
2016年的研究实在小鼠胚胎期进行敲除,可能影响了小鼠的发育,导致表型有所偏差。可是这一模型也有优势,NAD+水平是逐渐降低的,能够模拟渐进式衰老的表型。
相反,2025年的研究用的成年期小鼠肌肉有一定耐受性,会造成NAD+水平断崖式下降,不符合正常衰老的认知。
所以,科学研究就是这样,可能条件发生微小的改变,就会得出完全相反的结论,科学本就是百家争鸣,任何新的发现都需要被不断地验证和修正,不能因一项研究否定其整体价值。
同样实验内容,为何结论完全相反?
卡尔·萨根有一句名言,“超凡主张须有超凡证据”(Extraordinary claims require extraordinary evidence),这也是理性思考的一项重要原则。
正因如此,上面提到的完全相反的结论,也深深地引起了我们的兴趣。长寿之家Changshou.com的专家团队在仔细研究讨论后认为,这项研究中也存在很多可讨论的空间和一些局限性。
第一,实验材料可能干扰了结果。制备NAMPT敲除鼠时用到了他莫昔芬(Tamoxifen)短期诱导Cre重组酶,已知他莫昔芬已被报道可激活AMPK、抑制mTOR通路[2],还被证实可以延长小鼠寿命[3],且剂量都是2mg/天,这可能掩盖了NAD+耗竭的负面影响。
(基于这一点我们也邮件咨询了作者特雷拜克博士,他认为他们使用他莫昔芬干预的时间很短,所以大概率没有影响;同时,他们对于野生型小鼠也做了同样的干预。)
第二,急性NAD+耗竭不同于自然衰老。实验中NAD+在短时间内骤降85%,而自然衰老中的NAD+水平缓慢下降(数十年降低30%-50%),两者的影响机制可能不同。
第三,单一器官实验结果不能代表全身情况。
为什么敲除一个NAD+的合成通路,可能不太会影响最终的肌肉表现?
我们通过一个简单的例子来说明:
一个人意外摔断了一颗牙齿,发现还能正常吃饭,但这不意味着可以忽略其他牙齿的作用。
要搞清楚原因,我们要了解关于NAD+合成代谢的两个关键事实:
• 器官分工不同
肝脏就像NAD+的“中央工厂”,负责生产原料供应全身[14];骨骼肌更像是“地方分厂”,主要自给自足;即使关掉肌肉的NAD+生产线,其他器官会立即补位,不会导致全身NAD+水平失衡,但不代表全身NAD+水平不重要。
• 人体神奇的代偿能力
《细胞·代谢》在上述论文发布后的第二天发表的另一项研究似乎就部分解释了一定原因——在肝脏中敲除NMNAT1(NAD+三条合成通路关键酶),也就是把肝脏的NAD+生产线几乎完全关闭后,肾脏立刻变身“替补队员”,接管了NAD+供应任务[6]。
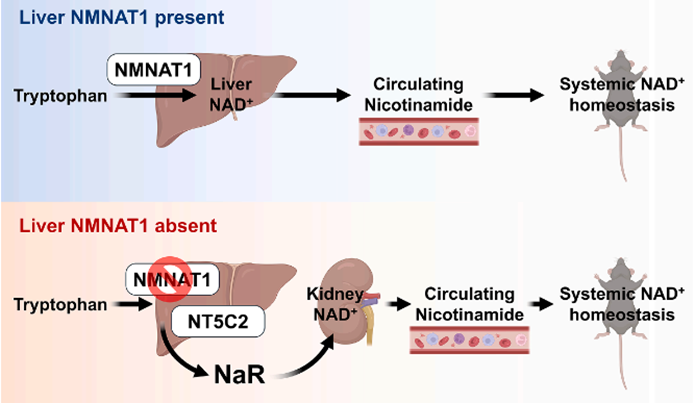
这说明我们身体具有强大的备用方案,更说明了单一器官实验不能代表全身情况。
误解背后的真相:NAD+的抗衰延寿逻辑梳理
除了对研究本身的误读外,铺天盖地的营销文还忽略了NAD+的背后抗衰延寿逻辑:
NAD+的合成和代谢是具有组织特异性的。虽然这项研究表明骨骼肌对NAD+波动具有较强的耐受性,但这并不意味着全身组织都是如此。NAD+在不同组织中扮演着不同的角色,在神经元等高度依赖NAD+的细胞中,对NAD+的需求可能与骨骼肌完全不同。
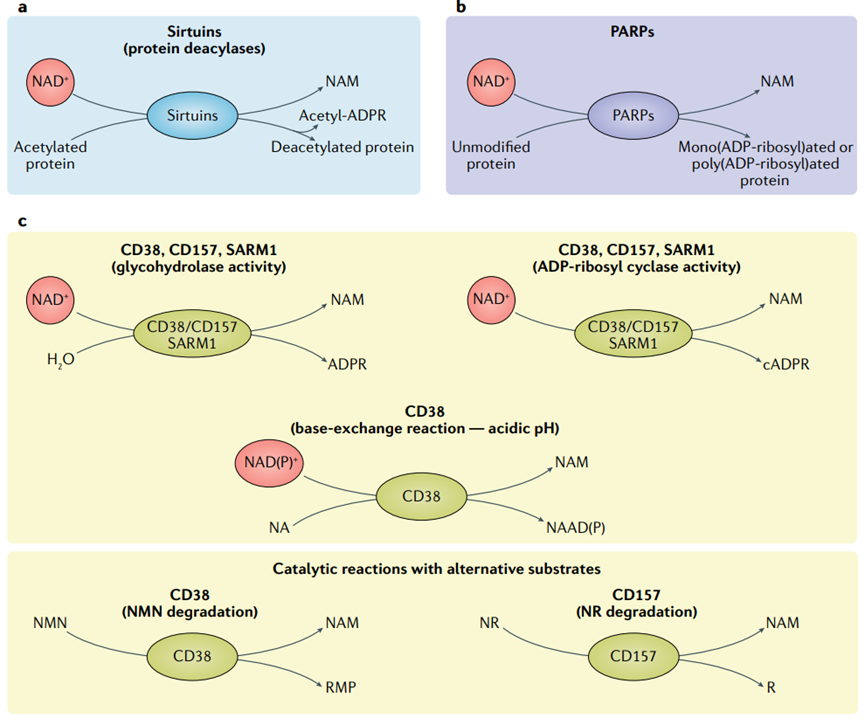
NAD+的作用机制不仅依赖于绝对浓度。它的本质是辅酶,可以激活许多重要的酶如Sirtuins、PARP、CD38等,这些酶在调控免疫反应、DNA 修复、细胞分裂、线粒体功能、表观遗传和氧化还原反应等方面起着重要作用[4]。
NAD+仍然重要,科学需全面看待
虽然肌肉能扛住NAD+减少,但这不意味着补充NAD+没用!这个逻辑的滑坡程度,基本上和“我能跑能跳——我比刘翔跨栏厉害”在一个幅度。
多年来,多项由不同国家、机构开展的不同类型研究都早已证实:人类NAD+水平会随着年龄的增长而自然下降[7,8]。
科学事实摆在这里,NAD+下降与衰老的关联已有大量临床证据,补充NAD+前体(NR/NMN)在多项人体临床试验中,展示出改善身体功能[9]、改善睡眠[10]、血脂[11]、降低心血管疾病风险[12]、改善糖尿病患者胰岛素敏感性[13]等健康益处。
所以总结一下,这项研究就像发现"汽车少个雾灯还能开",但大多数人不会因此拆掉所有车灯吧!
NAD+仍然是抗衰老的明星分子,只是我们需要更精准地使用它。从最近接连发表的NAD+代谢机制研究就能看出,我们对于NAD+的了解也在逐渐的更进一步。
另外,科学研究是研究人员耗费多年的研究心血,对于科研文章的解读需谨慎,不能断章取义,为了流量成为“标题党”,不仅是在误导读者,也是对论文研究者和研究成果的不尊重!正确理解研究成果,尊重科学,才是我们应有的态度。
参考资料:
[1]Chubanava, S. et al. NAD depletion in skeletal muscle does not compromise muscle function or accelerate aging. Cell Metabolism doi:10.1016/j.cmet.2025.04.002.
[2]Daurio, N. A. et al. AMPK Activation and Metabolic Reprogramming by Tamoxifen through Estrogen Receptor–Independent Mechanisms Suggests New Uses for This Therapeutic Modality in Cancer Treatment. Cancer Research 76, 3295–3306 (2016).
[3]Wang, B. et al. Intermittent clearance of p21-highly-expressing cells extends lifespan and confers sustained benefits to health and physical function. Cell Metabolism 36, 1795-1805.e6 (2024).
[4]Covarrubias, A. J., Perrone, R., Grozio, A. & Verdin, E. NAD+ metabolism and its roles in cellular processes during ageing. Nature Reviews Molecular Cell Biology 22, 119–141 (2020).
[5]Frederick, D. W. et al. Loss of NAD homeostasis leads to progressive and reversible degeneration of skeletal muscle. Cell Metabolism 24, 269–282 (2016).
[6]Song, W.-S. et al. Nicotinic acid riboside maintains NAD+ homeostasis and ameliorates aging-associated NAD+ decline. Cell Metabolism (2025) doi:10.1016/j.cmet.2025.04.007.
[7]Palmer, R. D., Elnashar, M. M. & Vaccarezza, M. Precursor comparisons for the upregulation of nicotinamide adenine dinucleotide. Novel approaches for better aging. Aging Medicine 4, 214–220 (2021).
[8]McReynolds, M. R., Chellappa, K. & Baur, J. A. Age-related NAD+ decline. Experimental Gerontology 134, 110888 (2020).
[9]Yi, L. et al. The efficacy and safety of β-nicotinamide mononucleotide (NMN) supplementation in healthy middle-aged adults: a randomized, multicenter, double-blind, placebo-controlled, parallel-group, dose-dependent clinical trial. GeroScience 45, 29–43 (2022).
[10]Zhao, B., Liu, C., et al. Clinical observation of the effect of nicotinamide mononucleotide on the improvement of insomnia in middle-aged and old adults. American Journal of Translational Medicine, 6(4), pp. 167–176.
[11]Kimura, S. et al. Nicotinamide mononucleotide is safely metabolized and significantly reduces blood triglyceride levels in healthy individuals. Cureus (2022) doi:10.7759/cureus.28812.
[12]Katayoshi, T. et al. Nicotinamide adenine dinucleotide metabolism and arterial stiffness after long-term nicotinamide mononucleotide supplementation: a randomized, double-blind, placebo-controlled trial. Scientific Reports 13, (2023).
[13]Yoshino, M. et al. Nicotinamide mononucleotide increases muscle insulin sensitivity in prediabetic women. Science 372, 1224–1229 (2021).
[14]Clark, A. J., Saade, M. C. & Parikh, S. M. The significance of NAD+ biosynthesis alterations in acute kidney injury. Seminars in Nephrology 42, 151287 (2022).
